Abstract
Introduction: Patients with sickle cell disease (SCD) are at much higher risk for infections from encapsulated organisms, particularly Streptococcus pneumoniae (pneumococcus), Neisseria meningitidis (meningococcus), and Hemophilus influenzae. Vaccinations and prophylactic penicillin (for pneumococcus) have declined but not eliminated their incidence. We aim to study the SCD admissions with infections from above mentioned encapsulated organisms.
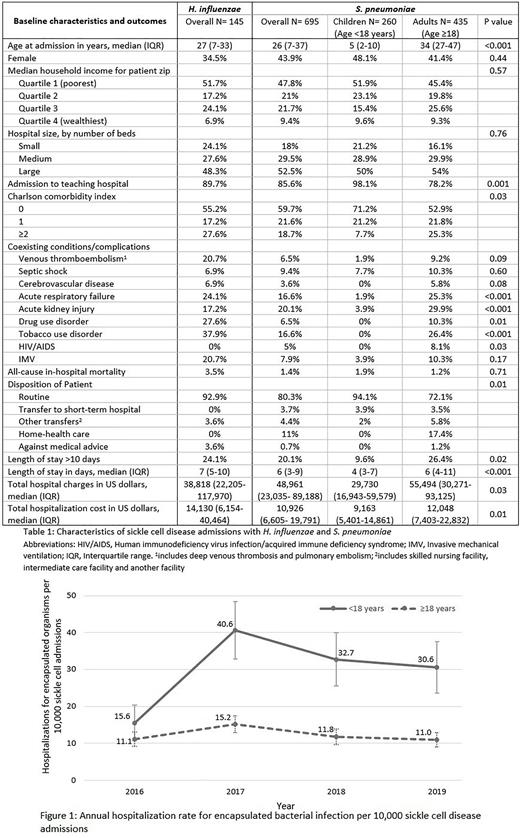
Methods: We performed a retrospective analysis using the National Inpatient Sample (NIS) database from 2016 to 2019 to identify SCD hospitalizations with either S. pneumoniae, N. meningitidis, or H. influenzae infections using appropriate International Classification of Diseases, Tenth Revision, Clinical Modification (ICD 10-CM) codes. SCD included HbSS (D57.0x), HbSC (D57.2x) and others (D57.1, D57.4x and D57.8x). Infections from S. pneumoniae and H. influenzae included sepsis (A40.3, A41.3), pneumonia (J13, J14), meningitis (G00.1, G00.0), and others (M00.1x, B95.3, A49.2, B96.3, and J20.1). N. meningitidis infections were identified by ICD-10-CM code A39.x. Admissions were divided into pediatric (<18 years) and adult (≥18 years) age groups and descriptive analysis was performed to compare demographics, hospital characteristics, and comorbid conditions/complications. We also calculated the annual hospitalization rate for encapsulated organisms per 10,000 SCD admissions. The methodology provided by the HCUP (Healthcare Cost and Utilization Project) was utilized, and weights were applied to produce national estimates.
Results: Out of 533,175 SCD admissions from 2016-2019, 830 (0.16%) had an infection from S. pneumoniae or H. influenzae. There were no admissions with N. meningitidis during our study period. The annual hospitalization rate for encapsulated bacterial infection per 10,000 SCD admissions ranged from 15.6/year to 40.6/year for the pediatric population and 11/year to 15.2/year among adults (Figure 1). Overall rate was 30 per 10,000 SCD admissions in pediatric population and 12 per 10,000 in adults (p <0.001).
Among S. pneumoniae infections, hospitalizations were highest for children ≤5 years at 64 per 10,000 SCD admissions, followed by 14 per 10,000 in children aged >5 & <18 years and lowest in adults (≥18 years) at 12 per 10,000 (p <0.001). Among 695 SCD admissions with S. pneumoniae, 325 (46.8%) were HbSS, and 65 (9.4%) had HbSC disease. Furthermore, 260 (37.4%) were <18 years and 435 (62.6%) were ≥18 years. The median age for children was 5 (2-10) years and 34 (27-47) for adults (p <0.001). Most admissions were males (56.1%), without significant comorbidities (Charlson comorbidity index 0 in 59.7%) and belonged to lowest income communities (47.8%). More than a quarter of adults (26.4%) had tobacco use disorder, and 8.1% had HIV/AIDS. Incidence of acute respiratory failure and acute kidney failure was higher in adults than in children (25.3% vs. 1.9%; p <0.001 and 29.9% vs. 3.9%; p <0.001 respectively). The median length of stay was 6 (4-11) days for adults and 4 (3-7) days for <18-year-olds (p <0.001). There were 26.4% adults compared to 9.6% children with a length of stay >10 days (p 0.02). Median hospital charges and costs were also higher for adults compared to children. Whereas there were no pediatric discharges requiring home health care, 17.4% of adults had home health care arranged (p 0.01). All-cause-in-hospital mortality was 1.4%.
Out of 145 H. influenzae admissions, 40 (27.6%) were <18 years, and 105 (72.4%) were ≥18 years. Like S. pneumoniae, the majority of SCD admissions with H. influenzae admissions were males (65.5%), belonged to the lowest income communities (51.7%), admitted to large (48.3%), teaching hospitals (89.7%), and had no significant comorbidities (Charlson comorbidity index 0 in 55.2%). Around 24.1% stayed in the hospital for >10 days, and 20.7% required invasive mechanical ventilation. The median length of stay was 7 (5-10) days, and all-cause-in-hospital mortality was 3.5% (Table 1).
Conclusion: Despite vaccinations and prophylactic penicillin, the burden of encapsulated bacterial infections in pediatric SCD hospitalizations remains disproportionately higher than in adults.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal